Degenerative disc disease (DDD) is a common condition influencing the spine, often associated with aging however also affected by lifestyle, genes, and injury. The spinal discs, situated in between vertebrae, act as cushions and shock absorbers, maintaining the spine's flexibility and allowing a variety of motion. Over time, these discs can undergo degeneration, leading to pain, stiffness, and limited mobility. While the term "disease" might suggest a progressive worsening, degenerative disc disease doesn't always deteriorate predictably; for some, symptoms may stabilize or improve over time.
One of the main contributors to disc degeneration is age. As we grow older, the spine's discs lose water content, becoming thinner and much less resistant. This dehydration can damage the architectural honesty of the disc, making it more at risk to damages. By the time most individuals reach their 30s or 40s, the damage on their spinal discs can begin to come to be recognizable. However, not every person will certainly experience pain or minimized function since the degree of discomfort varies extensively relying on everyone's special physiology and activity level.
Genetics also plays a significant duty in establishing whether somebody will develop DDD. Some people inherit a hereditary proneness to spine problems, which can manifest in the form of more fragile discs. Study has actually shown that families with a background of back concerns may hand down genes associated with disc degeneration. This predisposition does not ensure DDD, but it does increase the threat, particularly when integrated with lifestyle factors such as smoking, excessive weight, or participating in high-impact activities.
Injuries or recurring stress to the spine can also worsen the beginning of degenerative disc disease. Trauma, such as a loss or automobile accident, can hasten the malfunction of a spinal disc by disrupting its normal performance. People engaged in literally requiring work or sporting activities that put repetitive stress on the back, like hefty lifting or extreme operating, may also be at greater risk of creating DDD. The advancing effect of these activities can compromise the discs over time, leading to rips in the outer layer of the disc (the annulus fibrosus), making them more at risk to degeneration.
Pain is a main symptom associated with degenerative disc disease. However, the degree and location of pain can differ significantly depending on which part of the spine is affected. DDD can happen anywhere along the spine, but it's most generally seen in the cervical (neck) and lumbar (lower back) areas. Pain from DDD can range from mild to extreme and may be periodic or chronic. It often offers as a boring pain, acute pain, or burning feeling that radiates with nearby locations, consisting of the arms, shoulders, and legs, depending upon which disc is affected. This pain is generally worse when resting, bending, or turning and may be alleviated by relaxing or changing positions.
An additional symptom often associated with DDD is stiffness in the affected area. As the discs deteriorate, they lose height, leading to a constricting of the spaces in between the vertebrae. This loss of height lowers flexibility and movement, making day-to-day movements like flexing over or turning the neck unpleasant. Over time, the loss of disc height can also bring about additional issues such as nerve impingement. When a disc degenerates, it can bulge exterior or herniate, pressing versus neighboring nerves. This pressure on the nerves often causes pain, feeling numb, or tingling that can emit through the limbs, a condition referred to as radiculopathy.
Despite the discomfort, not all cases of degenerative disc disease need medical treatment. Treatment is often conventional, concentrating on pain management and enhancing capability through non-invasive techniques. Physical treatment, as an example, can be highly efficient in reinforcing the muscles surrounding the spine, assisting to sustain the affected discs. Workout and targeted stretching routines help improve flexibility and range of motion while minimizing rigidity and pain. Additionally, low-impact activities like strolling, swimming, and biking are often advised to maintain spinal health without putting excessive stress on the back.
Anti-inflammatory drugs and painkiller can help alleviate discomfort, especially during flare-ups. However, these are normally suggested for short-term relief, as prolonged use of medicines can bring about negative effects. In cases where pain is severe, and non-surgical treatments do not offer appropriate alleviation, spinal injections may be made use of. These injections commonly contain corticosteroids and anesthetics, which help reduce inflammation and numb the pain. However, like other treatments, spinal injections are not a cure for DDD and typically use short-lived alleviation.
When traditional approaches fail to control symptoms or when nerve compression leads to severe pain or motor weakness, surgery may be thought about. The surgical choices for degenerative disc disease vary, with the most common procedures being spinal fusion and synthetic disc replacement. Spinal combination includes joining two or more vertebrae together to reduce motion and stabilize the spine. Although effective oftentimes, this procedure may limit spinal flexibility. Alternatively, artificial disc replacement intends to maintain the spine's activity by changing the harmed disc with a prosthetic one, though it is not ideal for all individuals.
Degenerative disc disease can be handled and does not always imply a life of chronic pain. For many, lifestyle modifications play an important function in managing the condition. Maintaining a healthy weight helps reduce the lots on the spine, while giving up cigarette smoking enhances blood flow and, consequently, the supply of nutrients to the discs. Engaging in a normal workout regimen, focusing on strengthening core and back muscles, can improve spine security and reduce stress on the discs. For those that work in sedentary environments, making certain correct pose and taking routine breaks to stand or stretch can go a long way in maintaining spinal wellness.
Emotional aspects, such as stress and stress and anxiety, may also influence the assumption of pain. Mind-body strategies, including mindfulness, meditation, and cognitive behavior modification, are often utilized to help people manage chronic pain more effectively. Researches recommend that individuals that take part in these methods may experience less pain and boosted quality of life by learning to manage their body's feedback to discomfort.
Dealing with degenerative disc disease requires patience and flexibility. While no remedy exists, the range of treatments readily available enables many people to manage symptoms and maintain a top quality of life. The condition may change, with periods of extreme discomfort sprinkled with times of minimal symptoms. As scientific หมอนรองกระดูกเสื่อม research advances, treatments for DDD will remain to evolve, supplying intend to those affected by this common yet complex condition.
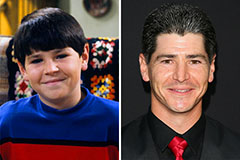 Michael Fishman Then & Now!
Michael Fishman Then & Now! Tina Louise Then & Now!
Tina Louise Then & Now! Bernadette Peters Then & Now!
Bernadette Peters Then & Now! Christy Canyon Then & Now!
Christy Canyon Then & Now! Dawn Wells Then & Now!
Dawn Wells Then & Now!